How AI Can Be Integrated Into Electronic Medical Records (EMRs) — Business Benefits and Technical Blueprint
The healthcare industry stands at a transformative crossroads. With over 90% of U.S. hospitals using Electronic Medical Records (EMR) and Electronic Health Records (EHR) systems, the foundation for digital healthcare is firmly established. Now, Artificial Intelligence is revolutionizing how these systems operate, transforming them from digital filing cabinets into intelligent clinical assistants that enhance care quality, reduce costs, and improve outcomes.
In 2025, 86% of healthcare organizations are extensively using AI, and the global AI in healthcare market is projected to reach $613.81 billion by 2034—a staggering growth from $26.69 billion in 2024. More importantly, healthcare organizations are seeing tangible returns: $3.20 for every $1 invested in AI, with typical ROI realized within just 14 months.
This comprehensive guide explores how AI integrates with EMR systems, the measurable business benefits, and the technical architecture required for successful implementation.
The EMR Challenge: Why AI Integration Is Essential
Before understanding AI integration, we must recognize the problems it solves. Despite digitizing patient records, most EMR systems create significant burdens:
The Clinical Documentation Crisis
Physicians spend 2-3 hours daily on documentation, time stolen from patient care. Traditional EMR systems require extensive clicking through screens, filling out templates, and repetitive data entry. This administrative burden contributes directly to:
- Physician burnout rates climbing to crisis levels
- Reduced patient interaction time
- Lower care quality due to exhausted clinicians
- Medical errors from data entry mistakes
- Staff turnover and retention challenges
The Data Utilization Gap
Healthcare organizations generate 50 petabytes of data annually (that’s 51 million gigabytes), yet most of this valuable information remains trapped in silos, underutilized for clinical decision-making. Traditional EMR systems store data but don’t analyze it, predict from it, or learn from it.
The Interoperability Problem
Patient information is scattered across labs, pharmacies, hospitals, and specialist offices. Without seamless integration, clinicians waste time manually gathering information, leading to:
- Delayed diagnoses and treatment
- Duplicate tests and procedures
- Inconsistent patient data
- Higher operational costs
AI integration addresses all these challenges while delivering measurable business value.
Understanding AI Integration in EMR Systems
What Does AI Integration Mean?
AI integration in EMR systems involves embedding machine learning algorithms, natural language processing (NLP), predictive analytics, and other AI technologies directly into electronic health record platforms. Rather than replacing EMR systems, AI enhances them with intelligent capabilities that:
- Automate routine tasks like data entry and documentation
- Analyze complex datasets to identify patterns and insights
- Predict patient outcomes and health risks
- Support clinical decision-making with evidence-based recommendations
- Personalize treatment plans based on individual patient profiles
- Optimize operations from scheduling to billing
Two Integration Architectures: Internal vs. External
Healthcare organizations can implement AI integration through two primary architectural approaches:
Internal Integration
Definition: AI models operate exclusively within the EMR vendor’s infrastructure, using their provided tools and platforms.
How It Works:
- EMR vendor (Epic, Cerner, Oracle Health, etc.) provides EMR AI development platforms
- Models are hosted on vendor servers
- All data processing occurs within the vendor’s secure environment
- Results are automatically filed back into patient records
Technical Implementation:
- Epic: Custom MUMPS routines or Epic’s AI integration tools
- Cerner: Integrated ML-based analytics through Cerner platforms
- Oracle Health: Built on Oracle Cloud Infrastructure with semantic AI foundation
- MEDITECH: Cloud-based AI integrations using MEDITECH’s framework
Advantages:
- Simplified security and compliance (vendor handles HIPAA requirements)
- Seamless integration with existing workflows
- Vendor support for troubleshooting and updates
- Lower infrastructure costs
Limitations:
- Less flexibility in model customization
- Vendor lock-in
- Limited control over model updates and features
- Potentially higher long-term costs
External Integration
Definition: Healthcare organizations host AI models outside the EMR system, maintaining control over the infrastructure and implementation.
How It Works:
- Research data warehouse pulls data from EMR
- External AI environment processes data and generates predictions
- Results are passed back to EMR through secure APIs
- Organization controls hosting, deployment, and model management
Technical Implementation:
- Custom-built AI servers or cloud platforms (AWS, Azure, Google Cloud)
- FHIR (Fast Healthcare Interoperability Resources) APIs for data exchange
- HL7 messaging standards for legacy system compatibility
- Secure data pipelines with encryption and authentication
Advantages:
- Complete control over model architecture and updates
- Flexibility for cutting-edge research and innovation
- Customization to specific organizational needs
- Multi-system integration across different EMR platforms
Limitations:
- Higher complexity in implementation
- Greater security responsibility (organization handles HIPAA compliance)
- Higher infrastructure costs
- Requires specialized technical expertise
Hybrid Approach: The Best of Both Worlds
Many successful implementations use a hybrid architecture, leveraging internal integration for core clinical workflows while maintaining external systems for specialized research and advanced analytics.
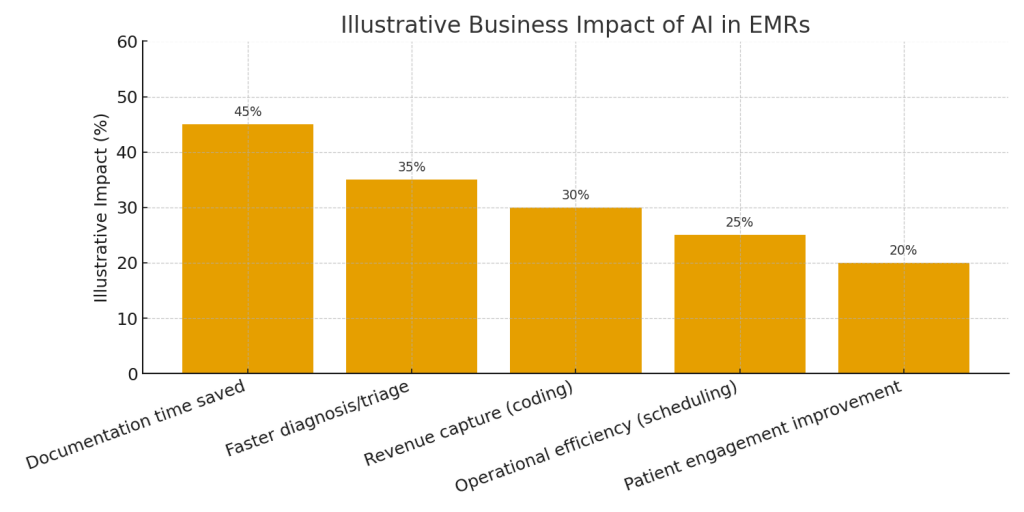
| Use case | Primary benefit | Business impact (illustrative) | Integration notes |
|---|---|---|---|
| AI-assisted clinical documentation | Reduce clinician documentation time; better coding | 45% time saved | ASR → clinical NLP → draft note in EHR; audit trail required |
| Real-time risk scoring (sepsis, deterioration) | Earlier interventions; fewer adverse events | 35% faster detection/triage | Trigger on vitals/lab events; tune thresholds to reduce alert fatigue |
| Imaging & pathology augmentation | Higher sensitivity; prioritized worklists | 30% throughput gain | DICOM/WSI ingestion → model inference → annotated images/reports |
| Revenue cycle & coding automation | Increase charge capture; reduce denials | 30% more accurate coding | NLP suggests codes; coder review & audit trail |
| Population health / care gap identification | Preventive care & guideline adherence | 20–30% screening improvement | Batch analytics with scheduled writes back to EMR |
The Business Case: Quantifiable Benefits of AI-Integrated EMR
Return on Investment (ROI)
The financial case for AI integration is compelling:
Direct Financial Returns:
- Average ROI: $3.20 for every $1 invested
- Payback period: 14 months on average
- Annual cost reduction: 35% within 18 months
- Mid-sized facilities savings: $2.4 million average
- Hospitals report: $3.20 return per dollar spent, often within 14 months
AI-driven automation could save the U.S. healthcare system over $150 billion annually by 2026 (Accenture, 2024).
1. Operational Efficiency Gains
Administrative Task Automation
Documentation Time Reduction:
- 50% reduction in documentation time with AI-powered transcription
- 2-3 hours daily saved per physician
- Therapists see three more patients per day without extending work hours
Clinical Workflow Improvements:
- Real-time voice-to-text transcription automatically formats SOAP notes
- AI extracts key details from conversations and updates charts automatically
- Progress notes generated in seconds rather than minutes
Real-World Example: A speech therapy clinic implemented AI-powered transcription in its EMR system, reducing documentation time by 50%, allowing therapists to see three additional patients per day without extending work hours.
Billing and Revenue Cycle Optimization
Error Reduction:
- 30% reduction in billing errors after AI-based coding integration
- Faster reimbursements through cleaner claims
- Fewer claim denials due to complete documentation before submission
Automated Medical Coding:
- AI assigns correct CPT codes based on treatment details
- Detects missing information before claim submission
- Verifies insurance eligibility in real-time
Financial Impact: A multidisciplinary therapy clinic reduced billing errors by 30% after integrating AI-based coding into its EMR system, leading to faster reimbursements and fewer claim denials.
Scheduling Optimization
No-Show Reduction:
- 20% reduction in no-show rates with AI-powered scheduling
- Analyzes patient behavior patterns to suggest optimal appointment times
- Sends automated reminders to improve compliance
Revenue Impact: A physical therapy practice using AI-powered scheduling tools saw a 20% reduction in no-show rates, leading to increased revenue and improved patient engagement.
2. Clinical Outcomes and Patient Care
Enhanced Diagnostic Accuracy
AI-Powered Clinical Decision Support:
- 42.7% improvement in identification accuracy with neural networks
- 58.4% reduction in false positives
- Real-time lab result analysis with pattern recognition
- Automated flagging of abnormalities correlated with patient histories
Medical Imaging AI:
- 90% of healthcare organizations use AI in radiology and imaging
- AI in medical imaging market valued at $1.76 billion in 2023
- Projected to exceed $20 billion by late 2020s
- Faster and more accurate detection of strokes, brain tumors, and breast cancer
Predictive Analytics for Proactive Care
Hospital Adoption:
- 65% of U.S. hospitals use predictive analytics or AI-driven predictive models
- 79% of these hospitals rely on predictive models embedded in their EHR systems
Patient Outcome Improvements:
- Early identification of patients at risk for complications
- Proactive intervention before health deterioration
- Personalized treatment plans based on individual health profiles
Real-World Impact: A neurorehabilitation clinic integrated AI into its EMR system to track motor function recovery in stroke patients. Results:
- 25% reduction in patient discharge delays
- Improved functional outcomes due to early intervention
- Better resource allocation based on AI predictions
Medication Safety and Adherence
Drug Interaction Prevention:
- AI monitors medication histories and cross-references allergies
- Automated alerts for potential drug interactions
- Predictive models forecast potential complications
- Proactive medication regimen adjustments
Adherence Monitoring:
- Automated reminders for missed doses
- Real-time tracking of medication compliance
- Early intervention for non-adherent patients
3. Enhanced Patient Engagement
AI-Powered Patient Portals
MyChart Assistant and Similar Tools:
- AI-powered chatbots provide instant answers to patient queries
- Pull appointment information, test results, and medical records on demand
- Offer guidance for common symptoms (sore throat, fever, etc.)
- Reduce call volumes to clinic staff by 30-40%
Wearable Device Integration
Real-Time Monitoring:
- AI detects movement patterns and tracks therapy progress
- Clinicians receive alerts if patient metrics decline
- Treatment plans adjusted remotely based on AI insights
Patient Outcomes: A hand therapy clinic used AI to monitor grip strength recovery in post-surgical patients. With real-time AI feedback, therapists adjusted home exercises, leading to a 15% faster return to daily activities.
Dropout Prevention
Engagement Strategies:
- AI analyzes patient dropout risks
- Personalizes engagement strategies for at-risk patients
- Sends motivational messages and escalates follow-ups automatically
4. Workforce Satisfaction and Retention
Burnout Reduction:
- 68% of physicians recognize advantages of AI in patient care (up from 63% in 2023)
- 57% say biggest opportunity is reducing administrative burden
- More time for patient interaction improves job satisfaction
- Lower turnover rates among clinical staff
Skill Enhancement:
- AI provides decision support, not replacement
- Clinicians make better-informed decisions with AI insights
- Continuous learning from AI recommendations
5. Population Health Management
Chronic Disease Management:
- AI monitors chronic conditions (diabetes, heart failure, COPD)
- Predicts exacerbations before they occur
- Enables proactive intervention and care coordination
Public Health Insights:
- Identifies disease outbreak patterns
- Tracks population health trends
- Supports preventive care initiatives
| Component | Purpose | Examples / Tools |
|---|---|---|
| Data ingestion & normalization | Collect FHIR/HL7/DICOM data; normalize codes & units | HAPI FHIR, Kafka, Debezium, DICOM routers |
| Feature store | Ensure parity between training & serving | Feast, Tecton, Redis/SQL-based store |
| Model training & registry | Versioned experiments and reproducible artifacts | MLflow, TensorFlow/PyTorch, experiment tracking |
| Model serving & MLOps | Low-latency inference, CI/CD for models | Triton, TorchServe, Seldon, SageMaker, Vertex AI |
| Explainability & audit | SHAP/LIME outputs mapped to clinical features; immutable logs | SHAP, custom explainers, ELK/Cloud logging, secure storage |
| Monitoring & retraining | Detect drift, performance drops, trigger retrain | Prometheus, Grafana, custom model health dashboards |
Core AI Technologies in EMR Integration
1. Natural Language Processing (NLP)
Applications:
- Clinical documentation: Converting conversations into structured notes
- Voice commands: “Show me patient’s recent lab results and current medications”
- Information extraction: Pulling key data from unstructured clinical notes
- Sentiment analysis: Identifying patient concerns and emotional states
Technical Stack:
- Large Language Models (GPT-4, Claude, specialized medical LLMs)
- Speech-to-text engines (Nuance, custom models)
- Entity recognition for medical terminology
- Context-aware processing for clinical relevance
Leading Implementations:
- Epic EHR: Azure OpenAI GPT-4 for natural language queries
- Oracle Health EHR: Voice-first solution with semantic AI foundation
- Stanford’s ChatEHR: Allows clinicians to “chat” with medical records
- Augmedix: Real-time doctor-patient talk conversion to medical notes
2. Machine Learning for Predictive Analytics
Use Cases:
- Readmission risk prediction: Identifying patients likely to return within 30 days
- Disease progression modeling: Forecasting diabetes, heart failure, etc.
- Treatment outcome prediction: Comparing patient profiles for optimal therapies
- Resource utilization forecasting: Predicting bed needs, staffing requirements
Technical Components:
- Supervised learning models trained on historical patient data
- Neural networks for complex pattern recognition
- Time-series analysis for longitudinal patient data
- Ensemble methods for improved accuracy
3. Computer Vision for Medical Imaging
Applications:
- Radiology: X-ray, CT, MRI analysis for abnormality detection
- Pathology: Microscopic image analysis for cancer detection
- Dermatology: Skin lesion classification
- Ophthalmology: Retinal imaging for diabetic retinopathy
Technical Architecture:
- Convolutional Neural Networks (CNNs)
- Transfer learning from pre-trained medical imaging models
- Real-time inference pipelines
- DICOM integration for medical imaging standards
4. Robotic Process Automation (RPA)
Administrative Automation:
- Insurance verification: Automated eligibility checks
- Claims processing: Submission and tracking without human intervention
- Appointment scheduling: Intelligent booking systems
- Data entry: Automated population of EMR fields
Business Impact:
- Tasks requiring hours of manual work completed in minutes
- Reduction in human error
- Improved staff productivity
Data Integration Strategies
FHIR (Fast Healthcare Interoperability Resources)
Why FHIR:
- Modern web API standard for healthcare data exchange
- Real-time data access and updates
- Widely supported by major EMR vendors
- Aligned with USCDI (U.S. Core Data for Interoperability)
Implementation:
FHIR Resources Used in AI Integration:
- Patient: Demographics and identifiers
- Observation: Lab results, vitals, clinical measurements
- Condition: Diagnoses and problems
- MedicationRequest: Prescriptions and medication orders
- DiagnosticReport: Imaging and lab report summaries
- Procedure: Surgical and therapeutic proceduresAuthentication:
- OAuth 2.0 flows for secure access
- Multiple flow types depending on use case
- Separate token acquisition logic for each flow
- HIPAA-compliant token handling
HL7 Messaging Standards
Use Case:
- Legacy system integration where FHIR isn’t available
- Real-time event notifications between systems
- Lab order placement and results retrieval
Message Types:
- ADT (Admission, Discharge, Transfer)
- ORM (Order messages)
- ORU (Observation results)
- SIU (Scheduling information)
API-Based Integration
Real-Time Capabilities:
- Instant data synchronization
- Bi-directional data flow
- Event-driven architecture with webhooks
- Queue-based processing for scalability
Technical Considerations:
- Rate limiting: Managing API quota efficiently
- Error handling: Retry logic and fallback mechanisms
- Latency optimization: Caching strategies and bulk operations
- Security: End-to-end encryption, token management
Cloud Infrastructure Requirements
Oracle Cloud Infrastructure (OCI)
Oracle Health EHR Built on OCI:
- Secure foundation leveraging AI for data organization
- Semantic AI foundation enabling contextual understanding
- Open system for extending agents and integrating third-party models
- Enterprise-grade performance and scalability
Microsoft Azure
Epic, eClinicalWorks, Allscripts Integration:
- Azure OpenAI platform for LLM integration
- HIPAA-compliant pipeline
- GPT-4 integration for natural language capabilities
- Cloud services supporting $100M+ investments
AWS and Google Cloud
Healthcare AI Infrastructure:
- Scalable compute for model training and inference
- HIPAA-eligible services and architectures
- Healthcare-specific data lakes
- Real-time analytics platforms
| Category | Example KPI | How to measure | Target (illustrative) |
|---|---|---|---|
| Clinical | Time to treatment (e.g., sepsis) | Pre/post implementation analysis from EHR timestamps | Reduce by 30–50% |
| Operational | Documentation time saved per clinician | Time-motion studies; EHR event logs | Reduce 30–45% per day |
| Financial | Charge capture increase / denial rate | Revenue cycle dashboard, claims analytics | Increase charge capture by 10–25% |
| Adoption & UX | Usage rate / acceptance of AI suggestions | Telemetry & clinician surveys | Adoption > 40% for targeted workflows |
| Safety | False positive / negative rates | Model monitoring + incident reports | Maintain low false negative rate; clinically acceptable thresholds |
Security and Compliance Architecture
HIPAA Compliance Requirements
Technical Safeguards:
- Data encryption: At rest and in transit (AES-256, TLS 1.3+)
- Access controls: Role-based access with least privilege
- Audit logging: Comprehensive tracking of all data access
- Authentication: Multi-factor authentication for all users
Business Associate Agreements (BAA):
- Comprehensive PHI protection clauses
- Liability coverage and breach notification procedures
- Vendor vetting and security assessments
Additional Regulatory Considerations
FDA AI/ML Pathway (2025):
- Regulatory framework for AI/ML-based software as medical device
- Continuous learning algorithms require ongoing validation
- Pre-determined change control plans
European Health Data Space (EHDS):
- EU regulations empowering individuals with health data control
- AI Act compliance for healthcare applications
- Cross-border healthcare AI standards
EU AI Act:
- Categorizes AI systems by risk level (unacceptable, high, limited, minimal)
- High-risk healthcare AI requires conformity assessments
- Mandatory documentation and audit trails
Performance Optimization
Model Inference Optimization
Latency Requirements:
- Clinical decision support: <500ms response time
- Documentation assistance: Real-time transcription
- Predictive analytics: Batch processing acceptable for non-urgent cases
Optimization Strategies:
- Model quantization for faster inference
- Edge computing for real-time applications
- Caching strategies for frequently accessed predictions
- Load balancing across multiple inference servers
Data Pipeline Efficiency
Bulk Data Operations:
- FHIR Bulk Export with
_sinceparameter for incremental updates - Reduces data transfer volumes by 70-90%
- Optimizes quota usage for large datasets
Event-Driven Architecture:
- Webhook systems for real-time notifications
- Queue-based processing to handle event surges
- Two-second response requirements for webhook events
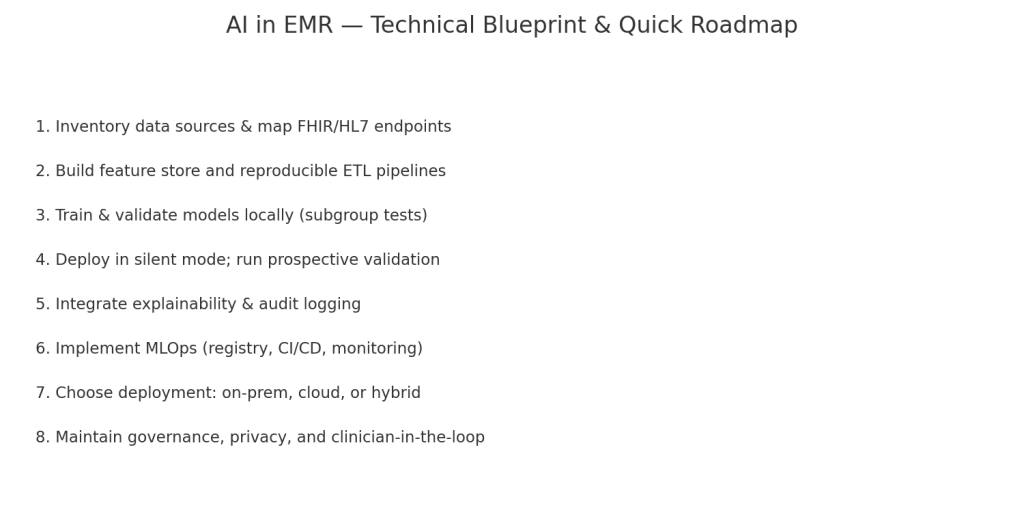
Step-by-Step Implementation Roadmap
Phase 1: Assessment and Planning (Weeks 1-4)
Week 1-2: Stakeholder Alignment
Objectives:
- Define clear business objectives and success metrics
- Identify clinical workflows for AI enhancement
- Secure executive sponsorship and budget approval
Key Activities:
- Conduct stakeholder interviews (clinicians, IT, administration)
- Document current pain points and inefficiencies
- Define ROI expectations and measurement methods
Week 3-4: Current State Assessment
Technical Evaluation:
- Data infrastructure: Assess EMR capabilities and data quality
- Integration readiness: Review API availability and documentation
- IT resources: Evaluate in-house technical capabilities
Compliance Review:
- HIPAA readiness assessment
- Data governance policies review
- Security framework evaluation
Budget Planning:
- Total cost of ownership (TCO) analysis
- Financial justification and ROI projections
Cost Ranges:
- Initial implementation: $20,000 – $1,000,000 (varies by scale and complexity)
- Annual licensing and support: 15-25% of initial cost
- Infrastructure maintenance: $5,000 – $50,000 monthly
Phase 2: Vendor Selection and Architecture Design (Weeks 5-8)
Vendor Evaluation Framework
Assessment Criteria:
- Technical Capability:
- AI model performance and accuracy
- Integration testing and compatibility
- Scalability to organizational needs
- Compliance and Security:
- HIPAA certification and audit reports
- Security controls and incident response
- Business Associate Agreement quality
- Business Factors:
- Transparent pricing model
- Vendor stability and track record
- Customer references and case studies
- Support quality and SLA commitments
Leading AI-EMR Vendors:
- Epic Systems: Comprehensive AI integration with Azure OpenAI
- Oracle Health: Next-generation cloud-native AI-driven EHR
- Cerner (Oracle Health): NLP and voice recognition integration
- eClinicalWorks: EVA AI assistant and ChatGPT integration
- Praxis EMR: Concept Processor AI that learns from usage
- MEDITECH: MyChart Assistant and clinician chatbots
- athenahealth: Nuance-powered AI documentation
Architecture Design
Internal vs. External Decision:
- Evaluate organizational technical capabilities
- Assess control requirements and compliance needs
- Consider long-term flexibility vs. implementation simplicity
Integration Patterns:
- FHIR API-first approach for modern interoperability
- HL7 messaging for legacy system compatibility
- Hybrid approach for complex environments
Scalability Planning:
- Design for horizontal scaling as usage grows
- Plan for multi-site deployment if applicable
- Consider disaster recovery and business continuity
Phase 3: Pilot Implementation (Weeks 9-16)
Pilot Scope Definition
Start Small:
- Select single clinical workflow or department
- Choose high-value, low-complexity use case
- Define clear success criteria
Common Pilot Use Cases:
- AI-powered clinical documentation in outpatient setting
- Predictive readmission alerts for specific condition
- Automated medical coding for one specialty
Technical Implementation
Data Pipeline Setup:
- Establish secure connections to EMR system
- Implement data validation and quality checks
- Configure real-time or batch data synchronization
Model Deployment:
- Deploy AI models to production environment (internal or external)
- Configure inference endpoints and APIs
- Implement monitoring and alerting
EMR Integration:
- Configure workflow integration points
- Set up user interfaces and alerts
- Implement result writing back to EMR
User Training and Change Management
Clinician Training:
- Hands-on workshops with actual system
- Documentation and quick reference guides
- Champions program for early adopters
IT Training:
- Technical architecture deep-dive
- Troubleshooting procedures
- Monitoring and maintenance protocols
Phase 4: Validation and Optimization (Weeks 17-20)
Performance Monitoring
Technical Metrics:
- Model accuracy and precision
- System latency and response times
- Error rates and failure modes
- API quota utilization
Clinical Metrics:
- Time savings for documentation
- Diagnostic accuracy improvements
- Alert appropriateness (false positive rates)
- User satisfaction scores
Optimization Cycle
Model Refinement:
- Retrain models with production data
- Adjust decision thresholds based on feedback
- Implement A/B testing for improvements
Workflow Adjustments:
- Refine integration points based on user feedback
- Optimize UI/UX for clinical efficiency
- Adjust alert frequencies and priorities
Phase 5: Full-Scale Deployment (Weeks 21+)
Rollout Strategy
Phased Approach:
- Department-by-department or site-by-site rollout
- Allow time for adjustment and feedback
- Maintain pilot group as expert resources
Communication Plan:
- Regular updates to all stakeholders
- Success stories and early wins shared broadly
- Transparent reporting of challenges and solutions
Ongoing Support
Help Desk Enhancement:
- AI-specific support procedures
- Escalation paths for technical issues
- User feedback collection mechanisms
Continuous Improvement:
- Quarterly performance reviews
- Regular model retraining cycles
- New use case identification and implementation
Real-World Success Stories
Case Study 1: Stanford Medicine’s ChatEHR
Challenge: Clinicians spent excessive time navigating EMR to find specific patient information.
Solution: Developed ChatEHR, allowing clinicians to ask questions in natural language: “What were this patient’s most recent lab results?” or “Summarize the entire patient chart.”
Implementation:
- Built using Large Language Models (LLMs)
- Integrated directly into Stanford’s EMR workflow
- Pulls data securely from patient records
- Provides contextually relevant answers
Results:
- Dramatically reduced time spent searching through EMR
- Improved clinician satisfaction with EMR usability
- Currently deployed to 33 physicians, nurses, PAs, and NPs for monitoring and refinement
Case Study 2: Neurorehabilitation Clinic – Stroke Recovery
Challenge: Difficulty identifying which stroke patients needed more intensive therapy vs. those ready for discharge.
Solution: Integrated AI into EMR to track motor function recovery patterns.
Implementation:
- AI analyzes patient progress data daily
- Compares against similar patient outcomes
- Flags patients needing intervention adjustments
- Recommends optimal discharge timing
Results:
- 25% reduction in patient discharge delays
- Improved functional outcomes through early intervention
- Better resource allocation based on AI predictions
Case Study 3: Speech Therapy Clinic – Documentation Automation
Challenge: Therapists spent 50% of their time on documentation instead of patient care.
Solution: Implemented AI-powered transcription and documentation in EMR.
Implementation:
- Real-time speech-to-text during therapy sessions
- AI automatically formats notes into SOAP structure
- Extracts key clinical details for chart updates
- Therapist reviews and approves in seconds
Results:
- 50% reduction in documentation time
- Three additional patients seen daily per therapist without extended hours
- Improved work-life balance and job satisfaction
Case Study 4: Multidisciplinary Therapy Clinic – Billing Optimization
Challenge: 30% error rate in medical billing leading to claim denials and delayed reimbursements.
Solution: Integrated AI-based coding into EMR system.
Implementation:
- AI assigns correct CPT codes based on treatment documentation
- Detects missing information before submission
- Verifies insurance eligibility in real-time
- Flags potential issues for human review
Results:
- 30% reduction in billing errors
- Faster reimbursements through cleaner claims
- Fewer claim denials due to complete documentation
Common Challenges and Solutions
Challenge 1: Data Quality and Standardization
The Problem: EMR data is often inconsistent, incomplete, or non-standardized, making AI training difficult.
Solutions:
- Data cleaning pipelines: Automated processes to identify and correct data quality issues
- Standardization efforts: Implement common data models (OMOP, FHIR resources)
- Data governance policies: Establish clear data entry standards and validation rules
- Incremental improvement: Start with highest-quality data sources and gradually expand
Challenge 2: Integration Complexity
The Problem: Healthcare IT environments are complex with multiple systems requiring integration.
Solutions:
- API-first approach: Prioritize modern FHIR APIs over legacy integration methods
- Integration platforms: Use specialized EMR integration tools (Redox, HealthGorilla)
- Modular architecture: Break integration into manageable components
- Expert partnerships: Work with experienced healthcare IT integration specialists
Challenge 3: Clinician Adoption Resistance
The Problem: Healthcare providers may be skeptical of AI or resistant to workflow changes.
Solutions:
- Early clinician involvement: Include end users in design and testing phases
- Clear value demonstration: Show tangible time savings and outcome improvements
- Champion programs: Identify early adopters to advocate for AI tools
- Gradual implementation: Start with opt-in pilots before mandatory rollout
- Continuous feedback: Regularly collect and act on user feedback
Challenge 4: Regulatory Compliance Uncertainty
The Problem: AI regulations in healthcare are evolving, creating compliance uncertainty.
Solutions:
- Stay informed: Monitor FDA, HHS, and international regulatory updates
- Conservative approach: Implement stronger safeguards than minimally required
- Legal consultation: Work with healthcare compliance attorneys
- Documentation: Maintain comprehensive audit trails and validation records
- Flexible architecture: Design systems that can adapt to changing requirements
Challenge 5: Cost Management
The Problem: AI implementation can exceed budget projections without careful management.
Solutions:
- Phased investment: Spread costs over time with staged implementation
- Hybrid approach: Use internal integration where cost-effective, external where necessary
- Vendor negotiation: Secure favorable pricing and SLAs
- ROI tracking: Continuously measure returns to justify ongoing investment
- Cloud optimization: Right-size infrastructure to avoid overprovisioning
Future Trends in AI-EMR Integration
1. Agentic AI Systems
What’s Coming: AI agents that can autonomously complete multi-step workflows.
Applications:
- Autonomous documentation: AI observes patient interactions and completes all charting
- Proactive care coordination: AI schedules follow-ups, orders tests, and manages referrals
- Treatment plan optimization: AI continuously adjusts care plans based on patient response
Timeline: Early implementations in 2025-2026 with broader adoption by 2027-2028.
2. Multimodal AI Integration
Capability: AI systems that process multiple data types simultaneously (text, images, audio, sensor data).
Use Cases:
- Comprehensive patient assessment combining vitals, imaging, labs, and symptoms
- Real-time clinical decision support using all available data sources
- Predictive models that incorporate genomic, environmental, and behavioral data
3. Federated Learning for Privacy-Preserving AI
Technology: Train AI models across multiple healthcare organizations without sharing patient data.
Benefits:
- Improved model accuracy through diverse training data
- Enhanced patient privacy protection
- Compliance with strict data sharing regulations
- Collaborative research without data centralization
4. Quantum Computing for Healthcare AI
Potential: Quantum algorithms for complex optimization problems in healthcare.
Applications:
- Drug discovery and molecular modeling
- Treatment optimization for complex diseases
- Real-time genomic analysis
- Advanced predictive modeling
Timeline: Experimental implementations 2026-2028, practical applications 2030+.
5. Ambient Clinical Intelligence
Vision: Healthcare environments where AI observes and documents naturally without clinician input.
Components:
- Room-based sensors and microphones
- Computer vision for patient observations
- Automatic documentation of entire encounters
- Real-time clinical guidance during patient visits
Current Status: Stanford, Epic, and others actively developing ambient solutions.
Conclusion: The Imperative for AI-Integrated EMR
The integration of Artificial Intelligence into Electronic Medical Records is no longer optional—it’s an operational imperative. Healthcare organizations that delay AI adoption risk falling behind in clinical outcomes, operational efficiency, and financial performance.
The business case is clear:
- $3.20 return for every $1 invested
- 14-month average payback period
- $150 billion annual savings potential for U.S. healthcare
- 35% cost reduction within 18 months
The clinical benefits are proven:
- 50% reduction in documentation time
- 25% faster patient recovery in monitored conditions
- 42.7% improvement in diagnostic accuracy
- 30% reduction in billing errors
The market momentum is undeniable:
- 86% of healthcare organizations extensively using AI
- $613.81 billion market size by 2034
- 66% of physicians actively using healthcare AI
- 340+ FDA-approved AI tools currently deployed
Getting Started: Your Next Steps
Immediate Actions:
- Assess your current EMR capabilities and AI readiness
- Define 2-3 high-value use cases for pilot implementation
- Engage stakeholders across clinical, IT, and administrative teams
- Research vendor options and schedule demonstrations
- Develop preliminary ROI projections and budget proposal
Within 90 Days:
- Select initial AI integration partners and vendors
- Design technical architecture (internal vs. external)
- Establish governance framework for AI oversight
- Launch pilot implementation in controlled environment
- Begin clinician training and change management
Long-Term Vision:
- Scale successful pilots across organization
- Continuously expand AI use cases based on ROI
- Build internal AI expertise and capabilities
- Stay current with regulatory changes and best practices
- Participate in industry collaboration and knowledge sharing
The transformation of healthcare through AI-integrated EMR systems is already underway. Organizations that embrace this change strategically—with clear objectives, strong technical foundations, and commitment to change management—will lead the industry in clinical excellence, operational efficiency, and patient satisfaction.
The future of healthcare is intelligent. The future is now. The question is: Will your organization lead or follow?