How to Develop a Telemedicine App
The COVID-19 pandemic has resulted in a fundamental shift in the way healthcare is delivered. In-person appointments are no longer possible or advisable in many cases, which has resulted in a surge in the use of telemedicine apps. Telemedicine apps allow patients to consult with their doctors remotely, using video, audio, or text chats.
If you’re a startup CEO, CIO, or CTO, you may be considering developing a telemedicine app for your company. But how do you go about doing that? In this blog post, we’ll take you through the steps you need to take to develop a successful telemedicine app.
Telemedicine apps market overview
The global telehealth apps market was valued at $6.24 billion in 2021 and is expected to grow at CAGR of 36.5% from 2022 to 2028, according to the Grand View Research. The growing adoption of smartphones and the availability of high-speed internet are the major factors driving the growth of the market.
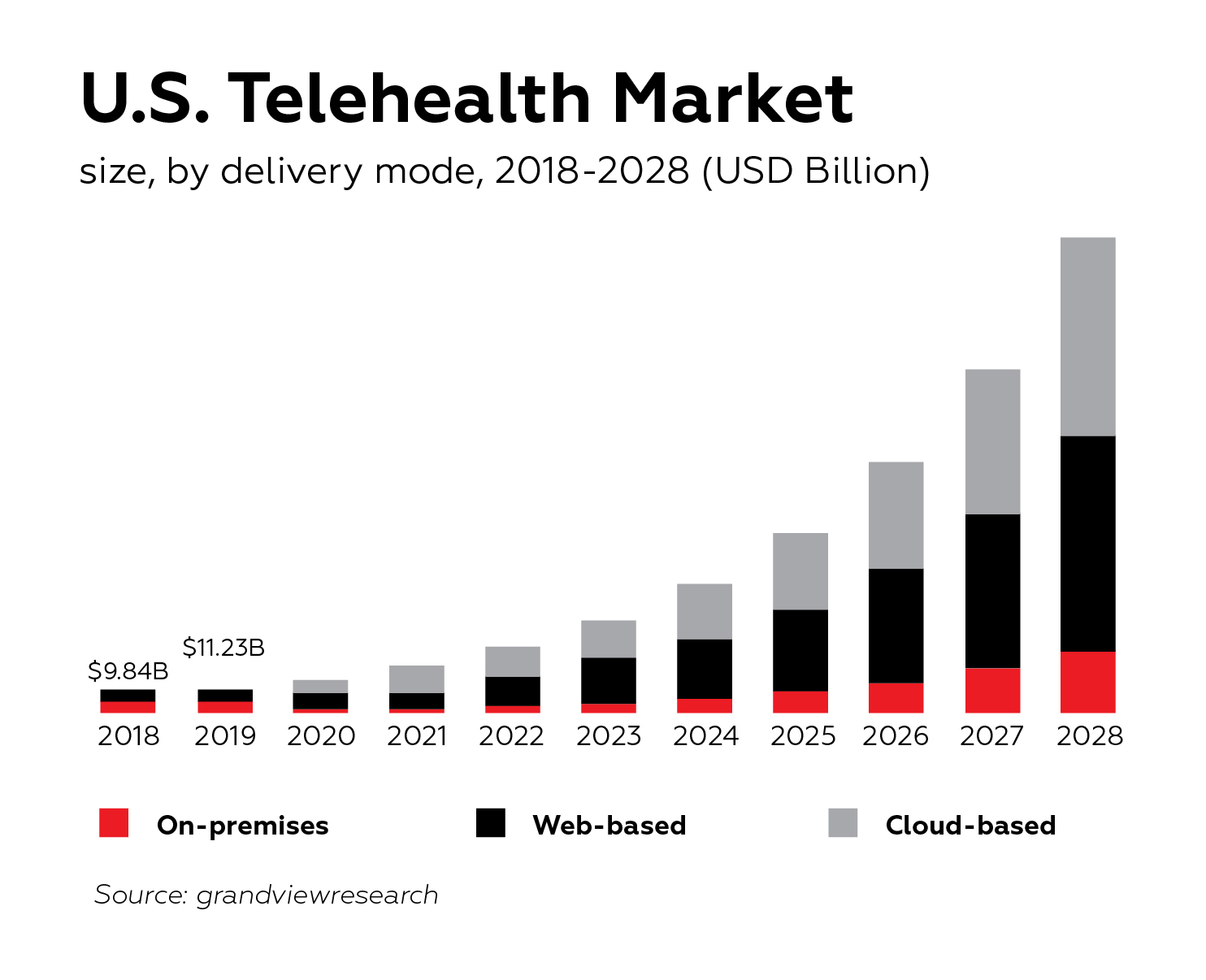
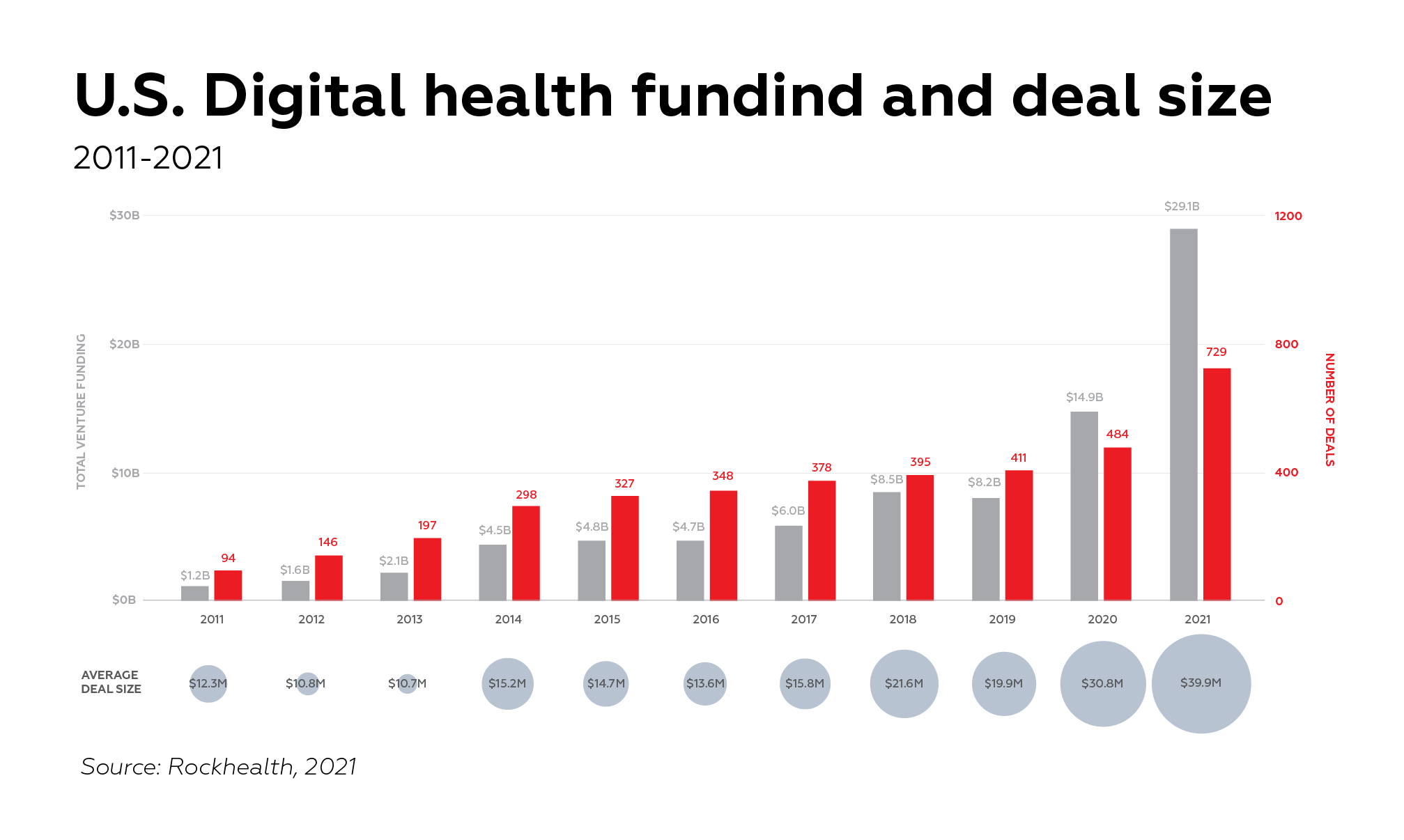
The COVID-19 pandemic has shown the potential of telemedicine and is expected to fuel the growth of the market in the coming years. The number of downloads for telemedicine apps increased manifold during the pandemic as people were confined to their homes and avoiding hospitals. It’s no wonder that digital health startups accumulated jaw-dropping $29.1 billion across 729 deals, with an average deal size of almost $40 million, according to Rock Health.
Top 5 benefits of telemedicine apps
Telemedicine apps provide many benefits both for doctors and their patients. Here are top 5 benefits of telemedicine apps:
Increases patient satisfaction
Patients can consult with doctors from the comfort of their homes without having to travel to clinics or hospitals. This is especially useful for people with chronic conditions who have to frequently visit doctors. With the help of these apps, patients can easily schedule appointments, view test results, and ask questions.
Improves access to care
Telemedicine apps can help improve access to care in remote and rural areas where patients have to travel long distances to see a doctor. It can also help patients who have difficulty getting to a doctor’s office due to their work schedule or other commitments.
Saves doctors’ time
Doctors can use telemedicine apps to quickly consult with patients and provide treatment. This saves time as patients do not have to come to the clinic or hospital for every small issue.
Makes work more efficient
Telemedicine apps also help medical organizations improve their workflow and efficiency. Given that telemedicine apps are easily integrated with existing internal systems like EMR software, doctors can quickly consult with patients, order tests, and receive results without having to physically visit each department.
Extends outreach
Telemedicine apps help hospitals by providing a new way to connect with potential clients. By offering a telemedicine app, hospitals can reach more people in a way that is convenient for them. This can expand the hospital’s outreach and help to bring in new patients.
Top 5 telemedicine apps
Lemonaid
Lemonaid is one of the most popular telemedicine apps in the US that provides primary healthcare services to a wide range of audiences. Lemonaid can easily connect patients with dozens of physicians and clinical support specialists. Importantly, prescriptions can also be delivered to local pharmacies, significantly simplifying prescription management for patients.
AmWell
AmWell focuses on fixed-cost, 24/7 medical consultation for urgent care, and can easily connect patients with therapists, psychiatrists, pediatrists, dermatologists, and other medical professionals in a matter of minutes. Amwell can be easily integrated with existing EHRs and patient portals, making it a popular choise among established healthcare institutions. Amwell has received cumulative $866m from 16 investors since its inception.
K Health
K Health’s unique value proposition is that artificial intelligence is a first point of contact for patients that can automatically assess a patient’s condition based on provided symptoms and determine if a doctor visit is necessary. Apart from standard telemedicine app features, K Health can also handle prescription refills.
Doxy.me
Doxy.me is an easy-to-use web-based only telemedicine app that handles secure phone and video appointments with certified physicians. While there is no support for iOS or Android, the app is free to use for communication via voice or video. Importantly, the app can also be run through healthcare providers’ own domains.
Teladoc
Teladoc was founded in 2002 and its Teladoc app remains one of the most downloaded telemedicine apps that provides remote care for the widest range of cases. From mental health to chronic condition management, Teladoc provides access to the top 5% of medical specialists in the US, which makes it stand out from the competition.
3 main challenges of telemedicine app development
Accessibility and ADA compliance
One of the key challenges in developing telemedicine applications is creating a user interface (UI) that is both easy to use and provides the functionality that both medical professionals and patients need. Given that telemedicine apps are often intended to be used by the least tech-savvy audiences, it’s paramount to ensure that the interface isn’t cluttered and intuitive.
For example, aging populations, which are one of the most important target audiences for telemedicine apps, can be reluctant to use the app with unfamiliar UI elements. This is why telemedicine app development is not the right opportunity to showcase UI design sophistication and innovation. According to the former Apple accessibility expert, Cezary Tomczyk, the absolute majority of telemedicine apps lack accessibility features. In a nutshell, in the telemedicine app development context, usability is directly correlated with care quality.
There are a few key considerations to keep in mind when designing an app that is accessible for everyone:
- Consider compatibility with screen readers as virtually impaired people rely on them to use digital apps.
- Ensure that there is a high contrast between background and text color as people with poor eyesight often struggle to distinguish an app’s elements.
- Colorblind users may have difficulty distinguishing between similar colors, so it’s important to use colors that are starkly different from one another. For example, red color that is often associated with errors may not be distinguishable for colorblind people.
- Make buttons as big as possible with sufficient touch targets. This is important for people with dexterity issues.
- Make onboarding as easy as possible with minimum forms and questionnaires to complete. People with literacy challenges can be reluctant to complete lengthy user forms.
Apart from these basic guidelines, we highly advise to follow Web Content Accessibility Guidelines (WCAG), which are internationally recognized.
Data privacy and security
The development of telemedicine applications poses a number of data security challenges. First and foremost, these applications must comply with the Health Insurance Portability and Accountability Act (HIPAA), which sets strict standards for the handling of protected health information (PHI). In addition, telemedicine apps must be designed to protect patient privacy and security, as well as to ensure the confidentiality of communications between patients and their healthcare providers.
One way to ensure data security in the development of telemedicine apps is to build encryption into every step of data transmission and storage. This means not just using secure connections and password protection, but also encrypting data at rest and during transfer. Another important aspect of data security is user education, as often data breaches are not due to technological failures but rather human error. Providing training on best practices for password management and data handling can go a long way towards preventing unauthorized access to sensitive information.
As we’ve outlined in our previous article on cloud-based EHR systems, collaborating with a reliable cloud system provider can significantly alleviate the risks associated with data privacy and security.
Regulatory approval
Developing a telemedicine app can be a daunting task, as it often requires obtaining regulatory approval from regulatory authorities like FDA. The process of obtaining such approval can be long and arduous, as it involves ensuring that the app meets all applicable safety standards. When it comes to telemedicine app development, it’s imperative to understand what regulatory approvals you need to obtain.
For example, a telemedicine app that is intended to treat, diagnose, cure or prevent diseases without being part of a hardware medical device can be classified as Software as a Medical Device (SaMD) by FDA. Understanding whether your software falls under SaMD is a nuanced matter that often calls for expert opinion from an experienced healthcare software developer.
In reality, even the simplest, general-purpose telemedicine apps are classified as SaMD. For example, apps that collect patient data in real-time for the development of treatment plans, or use built-in accelerometer or hear-rate monitor on a smartphone to diagnose certain conditions are classified as SaMD.
Most important features in your telemedicine app
Doctor profile
A doctor should be able to easily add his or her credentials, years and areas of expertise, and appointment availability. One of the most crucial features here is to integrate a rating system that will encourage doctors to provide better care and help patients to be more confident in the choice of medical professional. Also, it’s important to implement a reliable online document verification system. We advise to use a third-party API-enabled software for that matter.
Patient history
Clear, error-free, and easily accessible patient history is one of the biggest prerequisites for improved patients’ outcomes. Based on test records, prescriptions, treatment history, and other patient data, doctors have a much better chance at making accurate treatment decisions. If possible, we suggest integrating existing EHR system as it can significantly lower development time and costs.
Digital prescriptions
Prescription management system is one of the most important features in a telemedicine app. It allows doctors to issue prescriptions directly from the app, which can then be filled at a local pharmacy. This eliminates the need to go to the doctor’s office in person and wait for a prescription to be issued.
A prescription management system would be especially useful for telemedicine apps that are used for chronic conditions, such as diabetes or asthma. In these cases, it is important for patients to have regular access to medication in order to manage their condition, without having to go through the hassle of scheduling an appointment with a doctor.
Appointment scheduling
Calendar integration and comprehensive scheduling appointment system is crucial. Ensure that patients can clearly see a doctor’s available time slots, can schedule appointment in as few clicks as possible, can easily reschedule if needed, and can be notified prior to the appointment.
Video conferencing
Secure and reliable video conferencing platform is at the heart of every value-adding telemedicine app. The platform has to be high quality, low latency, secure, and easily accessible by less tech-literate populations.
Given that telemedicine video conferencing implies the sharing of highly sensitive patient data, real-time video communication has to adhere to HIPAA. Instead of using conventional matching password method, we highly suggest to integrate biometric-based authentication methods like fingerprints or voice recognition.
External device integration
In many cases, to bring real value from a telemedicine app, it needs to be integrated with some sort of medical device like glucose meter, ECG patch, heart monitor device, or any other remote patient monitoring device. Such apps are considerably more costly to develop, more complicated in terms of regulatory approval, but can win over a narrower target audience and realize more revenue in the long-term.
Developing a telemedicine app step-by-step
- Figure out what problem you’re trying to solve.
The first step in any good software development project is understanding what problem you’re trying to solve. What need does your app fill? What are your users looking for? A telemedicine app could fill any number of needs, from providing on-demand access to primary care physicians to offering specialist consultation for rare conditions. Once you know what problem you’re solving, you can move on to the next step.
- Research the competition.
Before you start development on your app, it’s important to understand what other options are available to your potential users. What features do they offer? How do they solve the user’s problem? What are their strengths and weaknesses? Knowing what’s already out there will help you determine what features your app needs to have in order to be successful.
- Choose your platform
When it comes to selecting a platform for a telemedicine app, there are several factors to consider. First, it’s important to assess the demographic of your target user base and their preference for mobile devices. For example, Android tends to have a larger market share globally, while iOS commands a majority in the US. It may also be wise to consider whether web or desktop options are necessary, as this can expand your potential reach to individuals without smartphones.
Another consideration is the capabilities and limitations of each platform: for example, iOS offers strong privacy features and compatibility with wearable devices, whereas Android allows for more customization and greater global reach. Ultimately, it’s important to weigh all these factors carefully in order to select the platform that best fits the needs of both your users and your telemedicine service.
- Look into regulatory compliance
Regardless of the type of a telemedicine app you want to create, you need to ensure compliance with industry standards like HL7, data privacy standards like HIPAA, and standard operating procedures used for SaMD registration. Failing to comply with these regulations can result in fines and penalties, and become detrimental to a business as a whole. This is why we highly suggest working with experienced provider with an extensive background in developing regulatory compliant telemedicine apps.
- Build your app!
This is where the rubber meets the road; it’s time to start writing code and building out the features of your app. This phase of development is all about taking your vision and turning it into a working prototype that you can use to test hypotheses and gather feedback from potential users. We highly suggest to consider the aforementioned development challenges, especially those concerning UI, accessibility, and data privacy. Don’t worry about making the perfect product at this stage; the goal is simply to get something up and running so you can start collecting data.
- Test, test, test.
Before releasing your app into the wild, it’s important to test it thoroughly on both real devices and emulators/simulators. Make sure all the features work as intended and that there are no major bugs or crashes. This step is crucial; if your app isn’t stable, users will quickly abandon it in favor of a better-performing competitor.
Conclusion
Telemedicine is here to stay, and developing a telemedicine app is a great way for startups to enter this growing market. By following these simple steps—understanding what problem you’re solving, researching the competition, choosing your platform and development tools—you can build a successful telemedicine app that meets the needs of both patients and doctors alike. Good luck!

