How Leading Medical Companies Transformed Healthcare Through AI: Success Stories and Results
The healthcare industry stands at the precipice of its most significant transformation since the discovery of antibiotics. Artificial Intelligence (AI) is no longer a futuristic concept confined to research laboratories—it has become an integral component of modern medical practice, fundamentally reshaping how we diagnose diseases, develop treatments, and deliver patient care.
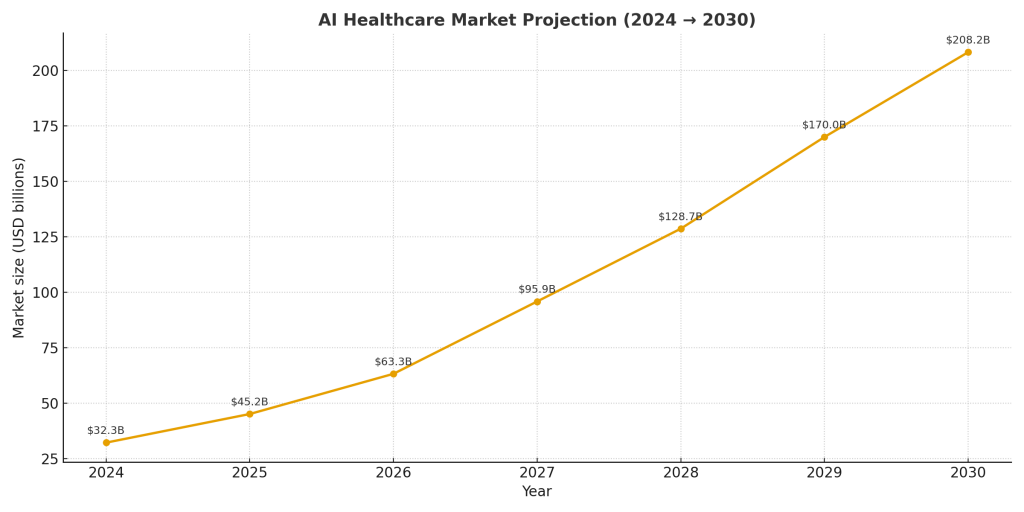
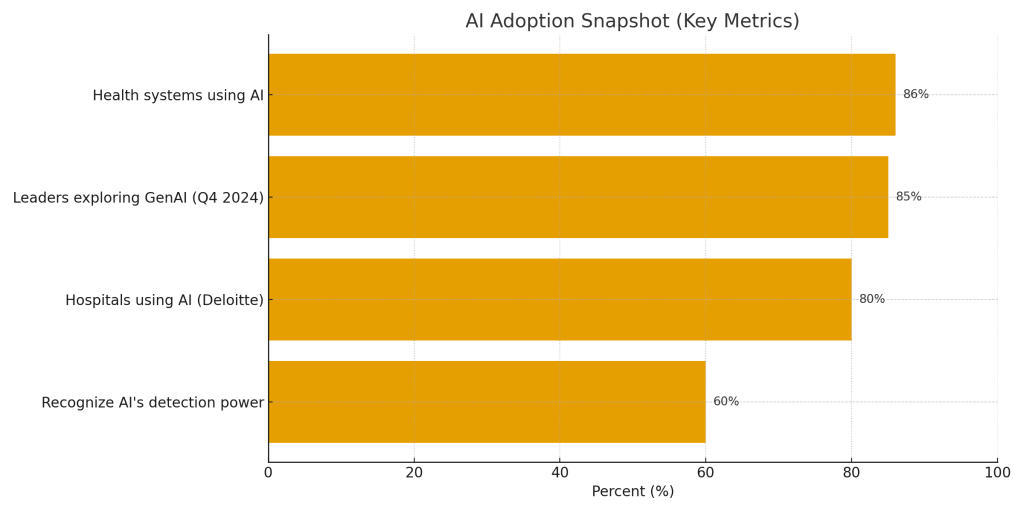
The numbers tell a compelling story: between 2024 and 2030, the AI healthcare market is projected to grow by 524% from $32.3 billion to $208.2 billion. More remarkably, 86% of health systems already leverage AI in their medical organizations, with 60% recognizing its ability to uncover health patterns and diagnoses beyond human detection.
But statistics alone don’t capture the human impact of this technological revolution. Behind every percentage point of growth lies a patient whose cancer was detected earlier, a physician whose diagnostic accuracy improved, or a hospital that reduced operational costs while simultaneously enhancing care quality.
This article examines the pioneering medical companies that didn’t just adopt AI—they transformed their entire operational models around it. We’ll explore their journeys, analyze their results, and extract lessons that can guide the next wave of healthcare innovation.
The Current State of AI in Healthcare
Before diving into specific company case studies, it’s essential to understand the broader landscape of AI adoption in healthcare.
Market Growth and Adoption Rates
The AI healthcare revolution is accelerating at an unprecedented pace. Between 2023 and 2024, the market size of AI in healthcare rose by 42%, with another 40% increase expected by 2025. This explosive growth reflects not just hype, but tangible value creation across the healthcare ecosystem.
In a survey conducted in Q4 2024, 85% of healthcare leaders from payers, health systems, and healthcare services companies were exploring or had already adopted generative AI capabilities. This represents a dramatic shift from mere experimentation to large-scale implementation.
Key Application Areas
According to Deloitte’s Health Care Outlook, 80% of hospitals now use AI to improve patient care and operational efficiency. AI is being deployed across multiple domains:
- Clinical Documentation: Over half of health systems report a high degree of success using AI for clinical documentation, with virtually all implementations using generative AI
- Diagnostic Support: Pattern recognition in medical imaging and pathology
- Administrative Efficiency: 92% of healthcare leaders believe Generative AI improves operational efficiency, while 65% see it as a tool for faster decision-making
- Patient Engagement: AI health assistants helping users track symptoms and manage chronic conditions
- Drug Discovery: Accelerating the identification of promising therapeutic compounds
The Impact on Outcomes
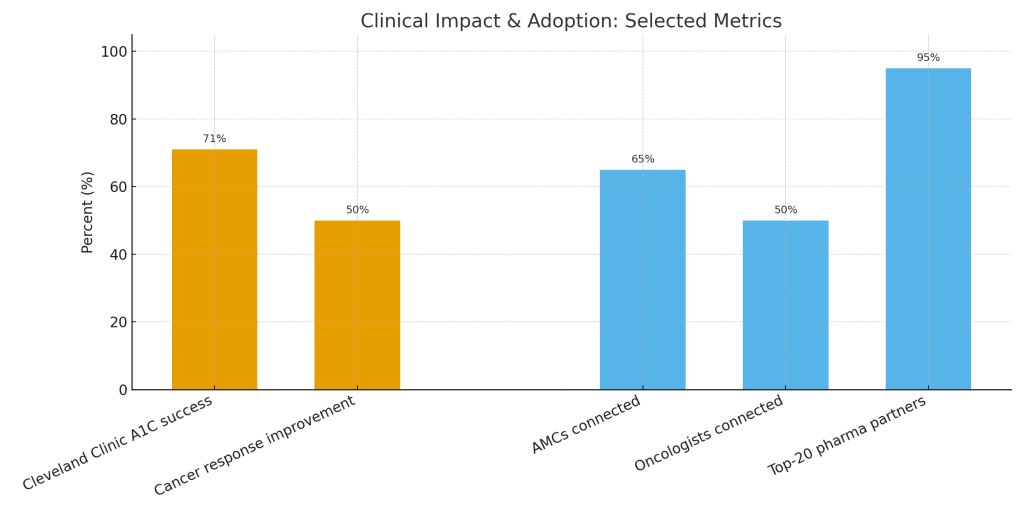
Perhaps most importantly, AI is delivering measurable improvements in clinical outcomes. Early adopters of AI systems report up to 50% response rate improvements in some cancer types, significantly higher than the 30-40% response rates typical of traditional targeted therapies.
Case Study 1: Tempus AI – Revolutionizing Precision Oncology
Company Overview
Founded in 2015 by Eric Lefkofsky, Tempus AI has emerged as one of the most successful examples of AI integration in healthcare. The company’s mission is audacious yet clear: to bring the power of artificial intelligence to healthcare by building the world’s largest library of clinical and molecular data and an operating system to make that data accessible and useful.
The Tempus Approach
Tempus built its platform around a fundamental insight: the key to precision medicine lies not just in sophisticated algorithms, but in the quality and scale of the underlying data. The company systematically collected, structured, and analyzed:
- Clinical data from electronic health records
- Molecular data from genomic sequencing
- Imaging data from radiology and pathology
- Treatment outcomes and patient responses
- Real-world evidence from actual clinical practice
This multimodal approach allowed Tempus to develop AI models that could identify patterns invisible to human clinicians, even highly trained oncologists.
Implementation Strategy
Tempus didn’t try to replace physicians; instead, it augmented their capabilities. The company’s AI platform provides oncologists with:
- Comprehensive Molecular Profiling: Advanced genomic sequencing that identifies actionable mutations and biomarkers
- Treatment Matching: AI-powered recommendations linking molecular profiles to appropriate targeted therapies and clinical trials
- Outcome Prediction: Models that forecast likely treatment responses based on similar patient profiles
- Real-World Evidence: Insights derived from analyzing thousands of similar cases
Measurable Results
The impact of Tempus’s AI implementation has been extraordinary:
Approximately 65% of all Academic Medical Centers in the US are now connected to Tempus, with over 50% of oncologists in the US connected through sequencing, clinical trial matching, and research-enabled partnerships. Additionally, 95% of the top 20 pharmaceutical oncology companies partner with Tempus.
These aren’t vanity metrics—they represent real-world adoption by the institutions and clinicians at the forefront of cancer care. The clinical outcomes have been equally impressive, with many cancer centers reporting improved patient matching to appropriate therapies and clinical trials.
The Paige Acquisition: Expanding AI Capabilities
In August 2025, Tempus made a strategic move that further solidified its position as an AI healthcare leader. Tempus acquired Paige, a company that developed and deployed several AI applications, including the first FDA-cleared AI application in pathology, for $81.25 million.
This acquisition was particularly significant because it brought Paige’s unparalleled dataset of 7 million de-identified cancer slides to Tempus, accelerating its mission of building the largest foundation model in oncology.
The Paige platform allows pathologists to detect cancer more accurately and efficiently, enabling care teams to make more precise and informed treatment decisions. By combining Paige’s digital pathology expertise with Tempus’s AI infrastructure, the company created a comprehensive oncology intelligence platform spanning genomics, imaging, and clinical data.
Key Success Factors
Several factors contributed to Tempus’s success:
- Data-First Strategy: Building the largest oncology data repository as the foundation for AI models
- Physician Partnership: Designing tools that augment rather than replace clinical judgment
- Regulatory Compliance: Navigating FDA requirements to gain clearances for AI applications
- Pharmaceutical Partnerships: Creating value for drug developers through real-world evidence generation
- Continuous Learning: Using outcomes data to continuously refine AI models
Case Study 2: Google Health and DeepMind – Bringing Tech Giant Resources to Healthcare
The Google Health Evolution
Google’s journey into healthcare AI represents the tech industry’s most ambitious and well-resourced attempt to transform medicine. Through Google Health and its AI research subsidiary DeepMind, the company has tackled some of healthcare’s most challenging problems.
Key AI Implementations
1. Diabetic Retinopathy Detection
One of Google Health’s most celebrated successes came in diabetic retinopathy screening. Published research shows that Google’s technology can identify signs of breast cancer as well as trained radiologists, and the company is now bringing this research to reality by partnering with iCAD to embed this technology in clinical settings.
The AI system was trained on thousands of retinal images and achieved performance comparable to ophthalmologists in detecting the disease. More importantly, it demonstrated the potential to extend specialist-level screening to underserved populations lacking access to ophthalmologists.
2. AlphaFold: Revolutionizing Protein Structure Prediction
Perhaps DeepMind’s most significant contribution to medicine has been AlphaFold, an AI system that predicts protein structures with remarkable accuracy. This breakthrough has profound implications for drug discovery and disease understanding, as protein structures determine how drugs interact with biological systems.
AlphaFold solved a 50-year-old grand challenge in biology, and DeepMind made the predictions for hundreds of millions of proteins freely available to researchers worldwide, accelerating scientific discovery across the field.
3. Med-Gemini: A Foundation Model for Medicine
Google Research advanced medical AI with Med-Gemini, a foundational model designed specifically for medical applications. This represents a shift from narrow, task-specific AI to more general-purpose medical intelligence that can handle diverse clinical scenarios.
Implementation Challenges and Lessons
Google’s healthcare journey hasn’t been without obstacles. While Google’s medical AI demonstrated super accuracy in laboratory settings, real-life clinical implementation proved more challenging. This highlighted a critical lesson: lab performance doesn’t automatically translate to clinical effectiveness.
The company learned that successful AI implementation in healthcare requires:
- Integration with existing clinical workflows
- User interface design optimized for busy clinicians
- Change management and training programs
- Addressing liability and responsibility questions
- Managing patient and provider expectations
Collaborative Approach
Recognizing these challenges, Google partnered with the Digital Medicine Society, Mayo Clinic, and others to create free resources helping health systems meaningfully invest and successfully implement AI. This collaborative approach acknowledges that transforming a $4.5 trillion industry requires more than just technology—it requires ecosystem-level cooperation.
Results and Impact
While Google’s healthcare initiatives have faced setbacks and course corrections, their impact is undeniable:
- AlphaFold’s protein structure predictions have been accessed millions of times by researchers
- Diabetic retinopathy screening algorithms are being deployed in developing countries
- Partnerships with health systems are gradually translating research into clinical practice
- The company’s research continues to push the boundaries of what’s possible with medical AI
Case Study 3: Cleveland Clinic – Academic Medical Center AI Leadership
Institution Profile
Cleveland Clinic, consistently ranked among the top hospitals in the United States, has distinguished itself not just in clinical care but in its aggressive adoption of AI technologies. As an academic medical center, it has the unique advantage of combining clinical excellence with research capabilities.
AI-Supported Precision Health Program for Diabetes
One of Cleveland Clinic’s most impressive AI implementations focused on Type 2 diabetes management. Research published in the New England Journal of Medicine Catalyst showed that 71% of study participants using the bundled AI-supported intervention system met the primary endpoint of achieving an A1C of 6.5% with fewer medications.
This result is remarkable for several reasons:
- Clinical Significance: Achieving tight glycemic control (A1C of 6.5%) typically requires escalating medication regimens. The fact that participants achieved this goal while using fewer medications represents a fundamental improvement in diabetes management.
- Holistic Approach: The program combined AI-driven insights with precision health coaching, demonstrating that the most effective implementations blend technology with human support.
- Reproducibility: The study was conducted with real patients in a clinical setting, not in controlled laboratory conditions, making the results more generalizable.
Implementation Framework
Cleveland Clinic’s approach to AI implementation offers lessons for other health systems:
1. Evidence-Based Adoption: Rather than implementing AI for its own sake, Cleveland Clinic rigorously evaluated which applications would deliver measurable clinical benefit.
2. Physician Engagement: AI tools were designed with input from clinicians who would actually use them, ensuring practical utility rather than theoretical sophistication.
3. Patient-Centered Design: The diabetes program incorporated patient preferences and lifestyle factors, recognizing that AI insights must translate into actionable changes patients can realistically implement.
4. Continuous Monitoring: Outcomes were systematically tracked, allowing for iterative improvements to the AI models and intervention protocols.
Broader AI Initiatives
Beyond diabetes, Cleveland Clinic has implemented AI across numerous domains:
- Predictive Analytics: Identifying patients at risk for deterioration or readmission
- Imaging Analysis: AI-assisted interpretation of cardiac imaging and radiology studies
- Operational Efficiency: Optimizing scheduling, staffing, and resource allocation
- Clinical Decision Support: Real-time alerts and recommendations integrated into electronic health records
Organizational Culture of Innovation
Cleveland Clinic’s success with AI stems partly from its institutional culture. The organization:
- Invests heavily in data infrastructure and interoperability
- Provides protected time for physicians to engage in AI-related research and implementation
- Maintains partnerships with technology companies and academic institutions
- Balances innovation with rigorous evaluation of safety and effectiveness
- Communicates transparently about both successes and failures
Case Study 4: Mayo Clinic – Building AI Governance and Implementation Frameworks
Mayo Clinic’s Strategic Approach
Mayo Clinic, one of the world’s most respected medical institutions, has taken a methodical approach to AI adoption that emphasizes governance, ethics, and systematic implementation.
The AI Implementation Playbook
Mayo Clinic partnered with the Digital Medicine Society and Google to help health systems find lasting benefit in AI through the creation of free implementation resources. This playbook addresses critical questions:
- How should health systems evaluate AI technologies?
- What governance structures are needed to ensure safe and effective AI deployment?
- How can AI implementations be sustained beyond pilot programs?
- What metrics should be used to assess AI’s impact on care quality and operational efficiency?
Key AI Applications
1. Cardiovascular AI
Mayo Clinic has been at the forefront of developing AI algorithms for cardiovascular medicine, including:
- ECG interpretation algorithms that can detect conditions like atrial fibrillation and left ventricular dysfunction
- Prediction models for cardiovascular events
- Imaging analysis tools for echocardiography and cardiac MRI
2. Pathology and Laboratory Medicine
The institution has deployed AI to enhance pathology services:
- Digital pathology platforms with AI-assisted diagnosis
- Laboratory test interpretation and correlation
- Quality control and error detection in lab processes
3. Clinical Operations
AI has been leveraged to improve healthcare delivery efficiency:
- Patient scheduling optimization
- Emergency department patient flow management
- Bed management and capacity planning
- Supply chain optimization
Governance and Ethics Framework
What distinguishes Mayo Clinic’s approach is its robust governance structure:
AI Governance Committee: Multi-disciplinary team overseeing AI initiatives Ethics Review: Formal process for evaluating AI implementations from ethical perspectives Bias Assessment: Systematic evaluation of AI models for potential biases Transparency Standards: Clear communication about when and how AI is being used in patient care
Measuring Success
Mayo Clinic has established comprehensive metrics for evaluating AI implementations:
- Clinical Outcomes: Changes in diagnostic accuracy, treatment effectiveness, and patient safety
- Operational Metrics: Efficiency gains, cost reductions, and workflow improvements
- User Satisfaction: Physician and patient experiences with AI-enhanced care
- Equity Measures: Ensuring AI benefits are distributed equitably across patient populations
Case Study 5: XpertDox – AI for Healthcare Operations
Company Overview
While many AI success stories focus on clinical applications, XpertDox represents a different but equally important use case: applying AI to healthcare’s notoriously complex administrative and operational challenges.
The Challenge: Revenue Cycle Management
Healthcare providers lose billions annually due to inefficient revenue cycle processes: incorrect coding, missed charges, delayed billing, and denied claims. These aren’t just financial issues—administrative burden contributes to physician burnout and diverts resources from patient care.
AI-Powered Solution
XpertDox developed AI systems to automate and optimize:
- Charge capture
- Medical coding
- Documentation quality
- Compliance monitoring
- Revenue cycle analytics
Remarkable Results at Nao Medical
The implementation at Nao Medical, a primary care provider, demonstrated the power of operational AI:
Post-implementation, Nao Medical saw a 15% jump in charge capture, a 60% improvement in quality code capture, and a 40% reduction in charge entry lag.
These aren’t marginal improvements—they represent transformative changes in revenue cycle efficiency. More importantly, they free clinical staff to focus on patient care rather than administrative tasks.
Rapid Growth and Validation
In 2023 and 2024, XpertDox more than doubled its client base each year, emphasizing responsible AI use in healthcare operations. This rapid growth validates both the technology’s effectiveness and the urgent need for AI solutions in healthcare administration.
Broader Implications
XpertDox’s success illustrates an important point: AI’s impact on healthcare extends far beyond diagnosis and treatment. Administrative AI can:
- Improve financial sustainability of healthcare organizations
- Reduce physician burnout by minimizing administrative burden
- Ensure appropriate reimbursement for care delivered
- Free resources that can be reinvested in patient care
- Improve compliance and reduce regulatory risk
Common Success Factors Across AI Implementations
Analyzing these diverse case studies reveals common elements that contribute to successful AI implementation in healthcare:
1. Data Quality and Infrastructure
Every successful implementation began with robust data infrastructure. High-quality, well-structured data is the foundation upon which effective AI models are built. Organizations that invested in:
- Electronic health record optimization
- Data standardization and interoperability
- Data governance and privacy protection
- Comprehensive data collection across the care continuum
…were better positioned to develop and deploy effective AI solutions.
2. Clinical Champion Engagement
AI implementations succeeded when they had physician champions who:
- Understood both clinical needs and technological possibilities
- Could bridge the gap between developers and end-users
- Provided feedback for iterative improvement
- Advocated for adoption among colleagues
Technology alone never drives transformation—people do. The most successful implementations prioritized human factors alongside technical capabilities.
3. Workflow Integration
AI tools that seamlessly integrated into existing clinical workflows were adopted; those that created additional work were abandoned. Successful implementations:
- Minimized disruption to established routines
- Provided value that justified any additional effort
- Offered intuitive interfaces requiring minimal training
- Delivered information at the point of care when decisions are made
4. Measurable Outcomes
Organizations that succeeded defined clear metrics for success before implementation and rigorously tracked outcomes. This approach:
- Justified continued investment in AI initiatives
- Identified areas needing improvement
- Demonstrated value to skeptical stakeholders
- Enabled continuous refinement of AI systems
5. Ethical Frameworks and Governance
Institutions that established robust governance structures for AI avoided pitfalls and built trust. Essential elements included:
- Transparent decision-making processes
- Bias detection and mitigation strategies
- Clear accountability for AI-assisted decisions
- Patient consent and communication protocols
- Regular audits of AI system performance
6. Interdisciplinary Collaboration
The most successful implementations brought together diverse expertise:
- Clinicians who understood medical problems
- Data scientists who built AI models
- Software engineers who created usable systems
- Implementation specialists who managed change
- Ethicists who considered implications
- Patients who provided user perspectives
7. Regulatory Navigation
Companies that succeeded understood and proactively addressed regulatory requirements:
- FDA clearance processes for medical devices
- HIPAA compliance for patient data
- Clinical validation requirements
- Documentation and audit trail creation
- Post-market surveillance protocols
Challenges and Lessons Learned
Even successful AI implementations faced significant challenges. Understanding these obstacles provides valuable lessons:
Technical Challenges
1. Data Quality Issues: Incomplete, inconsistent, or biased training data led to unreliable AI predictions. Solution: Invest heavily in data curation and validation.
2. Model Generalizability: AI systems trained on one population often performed poorly on others. Solution: Diverse training data and continuous monitoring across populations.
3. Integration Complexity: Connecting AI systems with existing IT infrastructure proved more difficult than anticipated. Solution: Allocate significant resources to integration and plan for longer implementation timelines.
Organizational Challenges
1. Change Resistance: Clinicians accustomed to traditional practices resisted AI-enabled workflows. Solution: Involve end-users early, demonstrate clear value, and provide comprehensive training.
2. Resource Constraints: AI implementation required significant financial and human resources. Solution: Start with focused pilot programs demonstrating ROI before scaling.
3. Skill Gaps: Few healthcare organizations had staff with both clinical and AI expertise. Solution: Invest in training existing staff and recruit hybrid talent.
Ethical and Social Challenges
1. Bias and Equity: AI systems sometimes perpetuated or amplified existing healthcare disparities. Solution: Systematic bias testing and diverse development teams.
2. Transparency and Trust: Black box AI models raised concerns about explainability. Solution: Develop interpretable AI and clear communication about how systems make recommendations.
3. Liability Questions: Determining responsibility when AI contributes to adverse outcomes remains unclear. Solution: Establish clear protocols, documentation, and legal frameworks.
The Future of AI in Healthcare
The success stories examined here represent only the beginning of AI’s transformation of healthcare. Looking forward, several trends will shape the next phase:
Expansion Beyond Pilot Programs
In 2025, healthcare organizations are expected to have more risk tolerance for AI initiatives, leading to increased adoption of solutions that meet business needs and bring ROI through increased efficiency or cost savings.
The shift from experimental pilots to production-scale implementations will accelerate, driven by proven results and competitive pressure.
Generative AI in Clinical Practice
Generative AI, exemplified by large language models, will transform clinical documentation, patient communication, and medical education. These systems can:
- Generate clinical notes from physician-patient conversations
- Answer patient questions with personalized, evidence-based information
- Summarize medical literature and guidelines for busy clinicians
- Create patient education materials tailored to individual health literacy levels
Multi-Modal AI Systems
Future AI systems will integrate diverse data types:
- Clinical notes
- Laboratory results
- Medical imaging
- Genomic data
- Wearable device data
- Social determinants of health
This holistic view will enable more accurate diagnosis, treatment selection, and outcome prediction.
Democratization of AI
As successful implementations prove themselves, AI will spread beyond elite academic medical centers to:
- Community hospitals
- Rural health clinics
- Developing countries
- Primary care practices
- Home healthcare
This democratization could help address healthcare disparities by extending specialist-level capabilities to underserved populations.
Regulatory Evolution
Regulatory frameworks will mature to balance innovation with safety:
- Streamlined approval pathways for low-risk AI applications
- Post-market surveillance requirements for AI systems
- Standards for validation and transparency
- International harmonization of AI regulations
Conclusion: Transformation Through Strategic AI Implementation
The medical companies profiled in this article share a common thread: they didn’t just adopt AI—they fundamentally reimagined how healthcare could be delivered. Their success offers several key takeaways:
1. AI is No Longer Experimental: With 86% of health systems already using AI and measurable improvements in clinical outcomes, AI has moved from research to standard practice.
2. Results Are Measurable and Significant: From 71% of diabetes patients achieving glycemic control goals to 50% improvements in cancer treatment response rates, AI is delivering tangible benefits.
3. Implementation Requires More Than Technology: Successful AI adoption demands data infrastructure, clinical champion engagement, workflow integration, and robust governance.
4. The Market Opportunity Is Enormous: With the healthcare AI market projected to reach $208.2 billion by 2030, companies that establish leadership now will shape the industry’s future.
5. Patient Impact Is the Ultimate Measure: Beyond efficiency gains and cost savings, AI’s true value lies in improved diagnoses, more effective treatments, and better patient outcomes.
The stories of Tempus, Google Health, Cleveland Clinic, Mayo Clinic, and XpertDox demonstrate that AI transformation is achievable, provided organizations approach it strategically. They invested in data infrastructure, engaged clinicians, measured outcomes rigorously, and remained committed despite challenges.
As we look to the future, the question is no longer whether AI will transform healthcare, but how quickly and equitably this transformation will occur. The pioneering companies examined here have shown the path forward. The next generation of healthcare leaders must build on their successes, learn from their challenges, and ensure that AI’s benefits reach all patients, regardless of geography, socioeconomic status, or institutional affiliation.
The AI revolution in healthcare is not coming—it’s here. The companies that embrace it strategically will lead the industry into a new era of precision, efficiency, and effectiveness in medicine. Those that delay risk being left behind in a rapidly evolving landscape where AI-enabled care becomes the standard, not the exception.
This article is based on published research, industry reports, and publicly available information about AI implementations in healthcare. As the field evolves rapidly, organizations should conduct thorough due diligence when evaluating AI technologies and implementation strategies.

